DEFINATION–
Vitiligo is a long-term problem in which growing patches of skin lose
their color. It can affect people of any age, gender, or ethnic group.
The patches appear when melanocytes within the skin die off. Melanocytes
are the cells responsible for producing the skin pigment, melanin,
which gives skin its color and protects it from the sun’s UV rays.
Globally, it appears to affect between 0.5 and 2 percent of people.
Fast facts on vitiligo
Vitiligo can affect people of any age, gender, or ethnicity.
There is no cure, and it is usually a lifelong condition.
The exact cause is unknown, but it may be due to an autoimmune disorder or a virus.
Vitiligo is not contagious.
Treatment options may include exposure to UVA or UVB light and depigmentation of the skin in severe cases.
VITILIGO
Vitiligo causes melanocytes to die, leaving patches of pale skin.
Vitiligo is a skin condition in which patches of skin loses their color.
The total area of skin that can be affected by vitiligo varies
between individuals. It can also affect the eyes, the inside of mouth,
and the hair. In most cases, the affected areas remain discolored for
the rest of the person’s life.
The condition is photosensitive. This means that the areas that are
affected will be more sensitive to sunlight than those that are not.
It is hard to predict whether the patches will spread, and by how
much. The spread might take weeks, or the patches might remain stable
for months or years.
The lighter patches tend to be more visible in people with dark or tanned skin.
CAUSES
The exact causes of vitiligo are unclear. A number of factors may contribute.
These include:
- an autoimmune disorder, in which the immune system becomes overactive and destroys the melanocytes
- a genetic oxidative stress imbalance
- a stressful event
- harm to the skin due to a critical sunburn or cut
- exposure to some chemicals
- a neural cause
- heredity, as it may run in families
- a virus
- Vitiligo is not contagious. One person cannot catch it from another.
It can appear at any age, but studies suggest that it is more likely to start around the age of 20 years.
SYMPTOMS
The only symptom of vitiligo is the appearance of flat white spots or
patches on the skin. The first white spot that becomes noticeable is
often in an area that tends to be exposed to the sun.
It starts as a simple spot, a little paler than the rest of the skin,
but as time passes, this spot becomes paler until it turns white.
The patches are irregular in shape. At times, the edges can become a
little inflamed with a slight red tone, sometimes resulting in
itchiness.
Normally, however, it does not cause any discomfort, irritation, soreness, or dryness in the skin.
The effects of vitiligo vary between people. Some people may have
only a handful of white dots that develop no further, while others
develop larger white patches that join together and affect larger areas
of skin.
TYPES
There are two types of vitiligo, non-segmental and segmental.
NON-SEGMENTAL VITILIGO
If the first white patches are symmetrical, this suggests a type of
vitiligo known as non-segmental vitiligo. The development will be slower
than if the patches are in only one area of the body.
Non-segmental vitiligo is the most common type, accounting for up to 90 percent of cases.
The patches often appear equally on both sides of the body, with some
measure of symmetry. They often appear on skin that is commonly exposed
to the sun, such as the face, neck, and hands.
Common areas include:
- backs of the hands
- arms
- eyes
- knees
- elbows
- feet
- mouth
- armpit and groin
- nose
- navel
- genitals and rectal area
However, patches can also appear in other areas
Non-segmental vitiligo is further broken down into sub-categories:
Generalized: There is no specific area or size of patches. This is the most common type.
Acrofacial: This occurs mostly on the fingers or toes.
Mucosal: This appears mostly around the mucous membranes and lips.
Universal: Depigmentation covers most of the body. This is very rare.
Focal: One, or a few, scattered white patches develop in a discrete area. It most often occurs in young children.
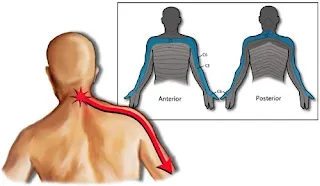
SEGMENTAL VITILIGO
Segmental vitiligo spreads more rapidly but is considered more constant
and stable and less erratic than the non-segmental type. It is much less
common and affects only about 10 percent of people with vitiligo. It is
non-symetrical.
It is more noticeable in early age groups, affecting about 30 percent of children diagnosed with vitiligo.
Segmental vitiligo usually affects areas of skin attached to nerves
arising in the dorsal roots of the spine. It responds well to topical
treatments.
COMPLICATIONS
Vitiligo does not develop into other diseases, but people with the condition are more likely to experience
painful sunburn
- hearing loss
- changes to vision and tear production
- A person with vitiligo is more likely to have another autoimmune
disorder, such as thyroid problems, Addison’s disease, Hashimoto’s
thyroiditis, type 1 diabetes, or pernicious anemia. Most people with
vitiligo do not have these conditions, but tests may be done to rule
them out.
OVERCOMING SOCIAL CHALLENGES
If the skin patches are visible, the social stigma of vitiligo can be
difficult to cope with. Embarrassment can lead to problems with
self-esteem, and in some cases, anxiety and depression can result.
People with darker skin are more likely to experience difficulties,
because the contrast is greater. In India, vitiligo is known as
“WHITE LEPROSY.”
Increasing awareness about vitiligo, for example, by talking to
friends about it, can help people with the condition to overcome these
difficulties. Connecting with other who have vitiligo may also help.
Anyone with this condition who experiences symptoms of anxiety and
depression should ask their dermatologist to recommend someone who can
help.
PHYSIOTHERAPY TREATMENT
Sometimes the best treatment for vitiligo is no treatment at all. In
fair-skinned individuals, avoiding tanning of normal skin can make areas
of vitiligo almost unnoticeable because the (no pigment) white skin, of
vitiligo has no natural protection from sun. These areas are easily
sunburned, and people with vitiligo have an increased risk to skin
cancer. They should wear a sunscreen with a SPF of at least 30 should be
used on all areas of vitiligo not covered by clothing. Avoid the sun
when it is most intense to avoid burns.
Disguising vitiligo with make-up, self-tanning compounds or dyes is a
safe, easy way to make it less noticeable. Waterproof cosmetics to
match almost all skin colors are available. Stains that dye the skin can
be used to color the white patches to more closely match normal skin
color. These stains gradually wear off. Self-tanning compounds contain a
chemical called dihydroxyacetone that does not need melanocytes to make
the skin a tan color. The color from self-tanning creams also slowly
wears off. None of these change the disease, but they can improve
appearance. Micropigmentation tatooing of small areas may be helpful.
If sunscreens and cover-ups are not satisfactory, your doctor may
recommend other treatment. Treatment can be aimed at returning normal
pigment (re-pigmentation) or destroying remaining pigment
(depigmentation). None of the re-pigmentation methods are permanent
cures.
TREATMENT OF VITILIGO DISEASE IN CHILDREN
Aggressive treatment is generally not used in children. Sunscreen and
cover-up measures are usually the best treatments. Topical
corticosteroids can also be used, but must be monitored. PUVA is usually
not recommended until after age 12, and then the risks and benefits of
this treatment must be carefully weighed.
REPIGMENTATION THERAPY
Topical Corticosteroids — Creams containing corticosteroid compounds can
be effective in returning pigment to small areas of vitiligo disease.
These can be used along with other treatments. These agents can thin the
skin or even cause stretch marks in certain areas. They should be used
under your dermatologist’s care.
PUVA
PUVA is a form of repigmentation therapy where a type of medication
known as psoralen is used. This chemical makes the skin very sensitive
to light. Then the skin is treated with a special type of ultraviolet
light call UVA. Sometimes, when vitiligo is limited to a few small
areas, psoralens can be applied to the vitiligo areas before UVA
treatments. Usually, however, psoralens are given in pill form.
Treatment with PUVA has a 50 to 70% chance of returning color on the
face, trunk, and upper arms and upper legs. Hands and feet respond very
poorly. Usually at least a year of twice weekly treatments are required.
PUVA must be given under close supervision by your dermatologist. Side
effects of PUVA include sunburn-type reactions. When used long-term,
freckling of the skin may result and there is an increased risk of skin
cancer. Because psoralens also make the eyes more sensitive to light,
UVA blocking eyeglasses must be worn from the time of exposure to
psoralen until sunset that day to prevent an increased risk of
cataracts. PUVA is not usually used in children under the age of 12, in
pregnant or breast feeding women, or in individuals with certain medical
conditions.
NARROW BAND UVB (NBUVB)
This is a form of photo-therapy that requires the skin to be treated
two, sometimes three, times a week for a few months. At this time this
form of treatment is not widely available. It may be especially useful
in treating children with vitiligo disease.
GRAFTING
Transfer of skin from normal to white areas is useful for only a small
group of vitiligo patients. It does not generally result in total return
of pigment in treated areas.
OTHER TRETMENT OPTION
Other treatment options include a new topical class of drugs called
immunomodulators. Due to their safety profile they may be useful in
treating eyelids and children. Excimer lasers may be tried as well.
DEPIGMENTATION THERAPY
For some patients with extensive involvement, the most practical
treatment for vitiligo disease is to remove remaining pigment from
normal skin and make the whole body an even white color. This is done
with a chemical called monobenzylether of hydroquinone . This therapy
takes about a year to complete. The pigment removal is permanent.