INTRODUCTION-
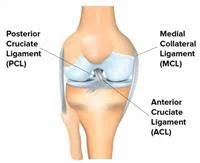
Your medial collateral ligament (MCL) is the knee ligament on the medial (inner) side of your knee connecting the medial femoral condyle and the medial tibial condyle. It is one of four major knee ligaments that help to stabilise the knee joint. It is a flat band of tough fibrous connective tissue composed of long, stringy collagen molecules.
The main function of the MCL is to resist valgus force, which occurs if the tibia/foot is forced outwards in relation to the knee.
ANATOMY OF MCL
CAUSES OF MCL INJURY
The MCL is injured when the (valgus) force is too great for the ligament to resist and the ligament is overstretched. This can occur through a sharp change in direction, twisting the knee whilst the foot is fixed, landing wrong from a jump, or the most common a blunt force hit to the knee, such as in football tackle. The incident usually needs to happen at speed. Muscle weakness or incoordination predispose you to a ligament sprain or tear.
SEVERITY OF MCL INJURY
The severity and symptoms of a knee ligament sprain depend on the degree of stretching or tearing of the knee ligament. You may notice an audible snap or tearing sound at the time of your ligment injury.
In a mild Grade I MCL sprain, the knee ligament has a slight stretch, but they don't actually tear. Although the knee joint may not hurt or swell very much, a mild ligament sprain can increase the risk of a repeat injury.
With a moderate Grade II MCL sprain, the knee ligament tears partially. Knee swelling and bruising are common, and use of the knee joint is usually painful and difficult. You may have some complaints of instability or a feeling of the knee giving way.
With a severe Grade III MCL sprain, the ligament tears completely, causing swelling and sometimes bleeding under the skin. As a result, the joint is unstable and can be difficult to bear weight. You may have a feeling of the knee giving way. Often there will be no pain or severe pain that subsides quickly following a grade 3 tear as all of the pain fibres are torn at the time of injury. With these more severe tears, other structures are at risk of injury including the meniscus and/or ACL.
DIAGNOSIS
On examination, your physiotherapist will look for signs of ligament injury. There will be tenderness over the ligament site, possible swelling and pain with stress tests. MRI may also be used to diagnose a knee ligament injury and look at other surrounding structures for combination injuries.
RECOVERY TIME
Treatment of an MCL injury varies depending on its severity and whether there are other combination injuries.
medial-collateral-ligament-grading-injuryGrade I sprains usually heal within a few weeks. Maximal ligament strength will occur after six weeks when the collagen fibres have matured. Resting from painful activity, icing the injury, and some anti-inflammatory medications are useful. Physiotherapy will help to hasten the healing process via electrical modalities, massage, strengthening and joint exercises to guide the direction that the ligament fibres heal. This helps to prevent a future tear.
When a Grade II sprain occurs, use of a weight-bearing brace or some supportive taping is common in early treatment. This helps to ease the pain and avoid stretching of the healing ligament. After a grade II injury, you can usually return to activity once the joint is stable and you are no longer having pain. This may take up to six weeks. Physiotherapy helps to hasten the healing process via electrical modalities, massage, strengthening and joint exercises to guide the direction that the ligament fibres heal. This helps to prevent a future tear and quickly return you to your pre-injury status.
When a Grade III injury occurs, you usually wear a hinged knee brace, locked into extension, and use crutches for 1-2 weeks to protect the injury from weight-bearing stresses. As pain resolves the brace can be unlocked to allow movement as tolerated. The aim is to allow for ligament healing and gradually return to normal activities. These injuries are most successfully treated via physiotherapy and may not return to their full level of activity for 3 to 4 months. All Grade III injuries should be rehabilitated under the guidance of your physiotherapist and knee specialist.
PHYSIOTHERAPY TREATMENT
Depending on the grade of injury you can start to feel better within days to just a few weeks of the injury. Your physiotherapy treatment will aim to:
1.Reduce pain and inflammation.
2.Normalise joint range of motion.
3.Strengthen your knee: esp quadriceps (esp VMO) and hamstrings.
4.Strengthen your lower limb: calves, hip and pelvis muscles.
5.Improve patellofemoral (knee cap) alignment
6.Normalise your muscle lengths
7.Improve your proprioception, agility and balance
8.Improve your technique and function eg walking, running, squatting, hopping and landing.
9.Guide return to sport activities and exercises
10.Minimise your chance of re-injury.
AIMS OF REHABILITATION-
The following examples are for information purposes only. We recommend seeking professional advice before attempting any rehabilitation. The aim of rehabilitation is to reduce pain and swelling, restore full mobility, improve strength and stability before a gradual return to full training.
GRADE 1 MCL INJURY
For a grade 1 MCL injury there may be mild tenderness on the inside of the knee over the ligament and usually no swelling. The rehabilitation guidelines for a mild medial ligament sprain can be split into 4 phases:
Phase 1: immediately following injury
Duration 1 week. Aims to reduce swelling if there is any, ensure the knee can be straightened fully and bent to more than 90 degrees and begin pain free strengthening exercises.
Rest from activities that cause pain. As pain allows, aim to walk normally without support or pain. Apply cold therapy and a compression support to limit any swelling. Apply ice for 15 minutes every 2 hours for the first day. The frequency can be gradually reduced to 3 times a day over the next few days. Do not apply ice directly to the skin as it may burn.
Sports massage techniques can usually be applied from day 2, specifically to the ligament. Ultrasound can also be applied to the ligament area. Maintain aerobic fitness with cycling. Apply cold therapy after each strengthening and stretching session.
Pain free stretching exercises for quadriceps and hamstring muscles as well as flexion and extension mobility exercises. Static strengthening exercises can begin as soon as pain allows. Isometric quadriceps exercises, calf raises with both legs and resistance band exercises for the hamstrings, hip abductors and hip extension but not for adduction as this will stress the medial ligament.
Phase 2: after 1 week
Duration 1 week. Aims - Eliminate any swelling completely, regain full range of movement, continue with strengthening exercises and return to slow jogging.
Rest from painful activities, however the athlete may be able to jog slowly as long as it is not painful. Apply cold therapy following exercise or rehabilitation exercises. Continue with stretching and strengthening exercises from phase 1.
Introduce dynamic strengthening exercises such as knee extension, knee flexion, half squats, step ups, single leg calf raise, bridging and leg press are suitable exercises if pain allows.
Cross friction massage to the ligament can be performed on alternate days. Maintain aerobic fitness with cycling, stepping machine and gentle jogging but no sudden changes of direction.
Phase 3: after 2 weeks
Duration 2 weeks. Aims to maintain full range of motion, equal strength of both legs, return to running and some sports specific training.
Continue to apply cold therapy after training sessions. Continue with sports massage techniques every 3 days. Continue with stretching exercises.
Build on dynamic strengthening exercises such as leg extension and leg curls exercises as well as squats to horizontal and lunges. Increase the intensity, weight lifted and number of repetitions. Aim for between 10 and 20 reps. Increase until the strength is equal in both legs.
In addition to straight running, start to include sideways and backwards running, agility drills and plyometric exercises. Increase speed to sprinting and changing direction drills.
Phase 4: after 4 weeks
Duration 3 to 6 weeks. Aims to return to full sports specific training and competition.
Sports massage for surrounding muscles on as weekly basis. Continue with strength training as above but start to include hopping and bounding exercises. The athlete should now be ready to gradually return to full sports specific training and then competition.
A knee support or a strapping / taping techniques may provide extra support on return to full training, however do not become reliant on this. It will weaken the joint. Use initially for confidence building.
GRADE 2 OR 3 SPRAIN-
For a grade 2+ and particularly 3 sprain it is important that the ends of the ligament are protected and left to heal without continually being disrupted. The rehabilitation guidelines for a grade 2+ or 3 medial ligament sprain (more severe) can be split into 4 phases:
Phase 1: immediately following injury
Duration 4 weeks. Aims to control swelling, maintain ability to straighten the leg bend the knee to more than 90 degrees, begin strengthening exercises.
Rest from all painful activities. Use crutches if necessary, non weight bearing to start with, then partial weight bearing from week 2 and by end of week 4 aim to be walking normally.
Wear a hinged or stabilised knee brace to protect the medial ligament. Apply cold therapy and compression. Apply ice / cold therapy for 15 minutes every 2 hours for the first 2 days and gradually reduce the frequency to 3 times a day over the next week. Pain free stretches for the hamstrings, quads, groin and calf muscles in particular. Mobility exercises should be done in the knee brace.
Sports massage (gentle cross frictions) may be possible from day 2 but allow a week for more severe injuries. As pain allows, static quads and hamstring exercises, double leg calf raises, hip abduction and extension. Knee extension mobility should only be to 30 degrees though. Maintain aerobic fitness on stationary cycle as soon as pain allows.
Phase 2: Following week 4
Duration 2 weeks. Aims to eliminate swelling, full weight bearing on the injured knee, full range of motion, injured leg almost as strong as the good one.
Continue with cold therapy and compression to eliminate swelling following exercises. Remove the knee brace at this stage. A simple stablized knee support is more suitable at this stage to apply compression to the knee. A therapist will continue with ultrasound and massage.
Range of motion exercises should continue along with isometric quadriceps exercises. Mini squats, lunges, double leg press, hamstring curls, step ups, bridges, hip abduction, hip extension and single leg calf raises can begin or be continued. It may be possible to begin to swim (not breaststroke!) or use stepper for aerobic fitness.
Phase 3: after week 6
Duration 4 weeks. Aims to regain full range of motion, strength, return to light jogging and by week 10 from injury, return to sports specific exercises.
Continue with cold therapy following training sessions. Wear a brace or support as required. Sports massage techniques to the ligament 2 to 3 times a weeks. Strengthening exercises as above increasing intensity and moving double leg exercises to single.
After week 6, no sooner, begin to run if comfortable, no sudden changes of direction though.
After week 8 begin to run sideways and backwards so by week 10 the athlete is able to begin to change direction at speed. For footballers, kicking may now be possible.
When confident enough plyometric drills, hopping, box jumps and agility drills can begin.
Phase 4: after week 10
Duration 2 to 4 weeks. Aims to return to full sports specific training and competition without a brace for support, full strength and mobility.
Gradually bring into training more and more sports specific drills, changing direction and plyometric, hopping and bounding exercises. Normal sports specific training can begin.
KNEE LIGAMENT SURGERY
Most MCL injuries resolve well with conservative management, however, surgery may be considered if there is significant ligament disruption eg Grade III. Surgery may also be required if the are significant combination injuries involving the ACL and/or meniscus. In these cases a knee specialist will guide the need for surgery.
Risks of surgery include infection, persistent instability and pain, stiffness, and difficulty returning to your previous level of activity. The good news is that better than 90% of patients have no complications post-surgery.
POST SURGICAL REHABILITATION
Post-operative knee rehabilitation is one of the most important aspects of knee surgery. The most successful and quickest outcomes result from the guidance and supervision of an experienced sports physiotherapist.
Your physiotherapy rehabilitation following knee surgery focuses on restoring full knee motion, strength, power and endurance. You'll also require balance, proprioception and agility retraining that is individualised towards your specific sporting or functional needs.
As mentioned earlier your sports physiotherapist is an expert in this field. We suggest you contact them for the best advice in your circumstances.
Your physiotherapist will guide your return to sport. It is highly variable and depends upon on your specific knee ligament injury and the demands of your demands of your sports.
PREVENTION OF RECURRENCE
A knee strengthening, agility and proprioceptive training program is the best way to reduce your chance of a knee ligament sprain. Premature return to high-risk activities such as sport are best discussed with your physiotherapist or surgeon.
Your medial collateral ligament (MCL) is the knee ligament on the medial (inner) side of your knee connecting the medial femoral condyle and the medial tibial condyle. It is one of four major knee ligaments that help to stabilise the knee joint. It is a flat band of tough fibrous connective tissue composed of long, stringy collagen molecules.
The main function of the MCL is to resist valgus force, which occurs if the tibia/foot is forced outwards in relation to the knee.
ANATOMY OF MCL
CAUSES OF MCL INJURY
The MCL is injured when the (valgus) force is too great for the ligament to resist and the ligament is overstretched. This can occur through a sharp change in direction, twisting the knee whilst the foot is fixed, landing wrong from a jump, or the most common a blunt force hit to the knee, such as in football tackle. The incident usually needs to happen at speed. Muscle weakness or incoordination predispose you to a ligament sprain or tear.
SEVERITY OF MCL INJURY
The severity and symptoms of a knee ligament sprain depend on the degree of stretching or tearing of the knee ligament. You may notice an audible snap or tearing sound at the time of your ligment injury.
In a mild Grade I MCL sprain, the knee ligament has a slight stretch, but they don't actually tear. Although the knee joint may not hurt or swell very much, a mild ligament sprain can increase the risk of a repeat injury.
With a moderate Grade II MCL sprain, the knee ligament tears partially. Knee swelling and bruising are common, and use of the knee joint is usually painful and difficult. You may have some complaints of instability or a feeling of the knee giving way.
With a severe Grade III MCL sprain, the ligament tears completely, causing swelling and sometimes bleeding under the skin. As a result, the joint is unstable and can be difficult to bear weight. You may have a feeling of the knee giving way. Often there will be no pain or severe pain that subsides quickly following a grade 3 tear as all of the pain fibres are torn at the time of injury. With these more severe tears, other structures are at risk of injury including the meniscus and/or ACL.
DIAGNOSIS
On examination, your physiotherapist will look for signs of ligament injury. There will be tenderness over the ligament site, possible swelling and pain with stress tests. MRI may also be used to diagnose a knee ligament injury and look at other surrounding structures for combination injuries.
RECOVERY TIME
Treatment of an MCL injury varies depending on its severity and whether there are other combination injuries.
medial-collateral-ligament-grading-injuryGrade I sprains usually heal within a few weeks. Maximal ligament strength will occur after six weeks when the collagen fibres have matured. Resting from painful activity, icing the injury, and some anti-inflammatory medications are useful. Physiotherapy will help to hasten the healing process via electrical modalities, massage, strengthening and joint exercises to guide the direction that the ligament fibres heal. This helps to prevent a future tear.
When a Grade II sprain occurs, use of a weight-bearing brace or some supportive taping is common in early treatment. This helps to ease the pain and avoid stretching of the healing ligament. After a grade II injury, you can usually return to activity once the joint is stable and you are no longer having pain. This may take up to six weeks. Physiotherapy helps to hasten the healing process via electrical modalities, massage, strengthening and joint exercises to guide the direction that the ligament fibres heal. This helps to prevent a future tear and quickly return you to your pre-injury status.
When a Grade III injury occurs, you usually wear a hinged knee brace, locked into extension, and use crutches for 1-2 weeks to protect the injury from weight-bearing stresses. As pain resolves the brace can be unlocked to allow movement as tolerated. The aim is to allow for ligament healing and gradually return to normal activities. These injuries are most successfully treated via physiotherapy and may not return to their full level of activity for 3 to 4 months. All Grade III injuries should be rehabilitated under the guidance of your physiotherapist and knee specialist.
PHYSIOTHERAPY TREATMENT
Depending on the grade of injury you can start to feel better within days to just a few weeks of the injury. Your physiotherapy treatment will aim to:
1.Reduce pain and inflammation.
2.Normalise joint range of motion.
3.Strengthen your knee: esp quadriceps (esp VMO) and hamstrings.
4.Strengthen your lower limb: calves, hip and pelvis muscles.
5.Improve patellofemoral (knee cap) alignment
6.Normalise your muscle lengths
7.Improve your proprioception, agility and balance
8.Improve your technique and function eg walking, running, squatting, hopping and landing.
9.Guide return to sport activities and exercises
10.Minimise your chance of re-injury.
AIMS OF REHABILITATION-
The following examples are for information purposes only. We recommend seeking professional advice before attempting any rehabilitation. The aim of rehabilitation is to reduce pain and swelling, restore full mobility, improve strength and stability before a gradual return to full training.
GRADE 1 MCL INJURY
For a grade 1 MCL injury there may be mild tenderness on the inside of the knee over the ligament and usually no swelling. The rehabilitation guidelines for a mild medial ligament sprain can be split into 4 phases:
Phase 1: immediately following injury
Duration 1 week. Aims to reduce swelling if there is any, ensure the knee can be straightened fully and bent to more than 90 degrees and begin pain free strengthening exercises.
Rest from activities that cause pain. As pain allows, aim to walk normally without support or pain. Apply cold therapy and a compression support to limit any swelling. Apply ice for 15 minutes every 2 hours for the first day. The frequency can be gradually reduced to 3 times a day over the next few days. Do not apply ice directly to the skin as it may burn.
Sports massage techniques can usually be applied from day 2, specifically to the ligament. Ultrasound can also be applied to the ligament area. Maintain aerobic fitness with cycling. Apply cold therapy after each strengthening and stretching session.
Pain free stretching exercises for quadriceps and hamstring muscles as well as flexion and extension mobility exercises. Static strengthening exercises can begin as soon as pain allows. Isometric quadriceps exercises, calf raises with both legs and resistance band exercises for the hamstrings, hip abductors and hip extension but not for adduction as this will stress the medial ligament.
Phase 2: after 1 week
Duration 1 week. Aims - Eliminate any swelling completely, regain full range of movement, continue with strengthening exercises and return to slow jogging.
Rest from painful activities, however the athlete may be able to jog slowly as long as it is not painful. Apply cold therapy following exercise or rehabilitation exercises. Continue with stretching and strengthening exercises from phase 1.
Introduce dynamic strengthening exercises such as knee extension, knee flexion, half squats, step ups, single leg calf raise, bridging and leg press are suitable exercises if pain allows.
Cross friction massage to the ligament can be performed on alternate days. Maintain aerobic fitness with cycling, stepping machine and gentle jogging but no sudden changes of direction.
Phase 3: after 2 weeks
Duration 2 weeks. Aims to maintain full range of motion, equal strength of both legs, return to running and some sports specific training.
Continue to apply cold therapy after training sessions. Continue with sports massage techniques every 3 days. Continue with stretching exercises.
Build on dynamic strengthening exercises such as leg extension and leg curls exercises as well as squats to horizontal and lunges. Increase the intensity, weight lifted and number of repetitions. Aim for between 10 and 20 reps. Increase until the strength is equal in both legs.
In addition to straight running, start to include sideways and backwards running, agility drills and plyometric exercises. Increase speed to sprinting and changing direction drills.
Phase 4: after 4 weeks
Duration 3 to 6 weeks. Aims to return to full sports specific training and competition.
Sports massage for surrounding muscles on as weekly basis. Continue with strength training as above but start to include hopping and bounding exercises. The athlete should now be ready to gradually return to full sports specific training and then competition.
A knee support or a strapping / taping techniques may provide extra support on return to full training, however do not become reliant on this. It will weaken the joint. Use initially for confidence building.
GRADE 2 OR 3 SPRAIN-
For a grade 2+ and particularly 3 sprain it is important that the ends of the ligament are protected and left to heal without continually being disrupted. The rehabilitation guidelines for a grade 2+ or 3 medial ligament sprain (more severe) can be split into 4 phases:
Phase 1: immediately following injury
Duration 4 weeks. Aims to control swelling, maintain ability to straighten the leg bend the knee to more than 90 degrees, begin strengthening exercises.
Rest from all painful activities. Use crutches if necessary, non weight bearing to start with, then partial weight bearing from week 2 and by end of week 4 aim to be walking normally.
Wear a hinged or stabilised knee brace to protect the medial ligament. Apply cold therapy and compression. Apply ice / cold therapy for 15 minutes every 2 hours for the first 2 days and gradually reduce the frequency to 3 times a day over the next week. Pain free stretches for the hamstrings, quads, groin and calf muscles in particular. Mobility exercises should be done in the knee brace.
Sports massage (gentle cross frictions) may be possible from day 2 but allow a week for more severe injuries. As pain allows, static quads and hamstring exercises, double leg calf raises, hip abduction and extension. Knee extension mobility should only be to 30 degrees though. Maintain aerobic fitness on stationary cycle as soon as pain allows.
Phase 2: Following week 4
Duration 2 weeks. Aims to eliminate swelling, full weight bearing on the injured knee, full range of motion, injured leg almost as strong as the good one.
Continue with cold therapy and compression to eliminate swelling following exercises. Remove the knee brace at this stage. A simple stablized knee support is more suitable at this stage to apply compression to the knee. A therapist will continue with ultrasound and massage.
Range of motion exercises should continue along with isometric quadriceps exercises. Mini squats, lunges, double leg press, hamstring curls, step ups, bridges, hip abduction, hip extension and single leg calf raises can begin or be continued. It may be possible to begin to swim (not breaststroke!) or use stepper for aerobic fitness.
Phase 3: after week 6
Duration 4 weeks. Aims to regain full range of motion, strength, return to light jogging and by week 10 from injury, return to sports specific exercises.
Continue with cold therapy following training sessions. Wear a brace or support as required. Sports massage techniques to the ligament 2 to 3 times a weeks. Strengthening exercises as above increasing intensity and moving double leg exercises to single.
After week 6, no sooner, begin to run if comfortable, no sudden changes of direction though.
After week 8 begin to run sideways and backwards so by week 10 the athlete is able to begin to change direction at speed. For footballers, kicking may now be possible.
When confident enough plyometric drills, hopping, box jumps and agility drills can begin.
Phase 4: after week 10
Duration 2 to 4 weeks. Aims to return to full sports specific training and competition without a brace for support, full strength and mobility.
Gradually bring into training more and more sports specific drills, changing direction and plyometric, hopping and bounding exercises. Normal sports specific training can begin.
KNEE LIGAMENT SURGERY
Most MCL injuries resolve well with conservative management, however, surgery may be considered if there is significant ligament disruption eg Grade III. Surgery may also be required if the are significant combination injuries involving the ACL and/or meniscus. In these cases a knee specialist will guide the need for surgery.
Risks of surgery include infection, persistent instability and pain, stiffness, and difficulty returning to your previous level of activity. The good news is that better than 90% of patients have no complications post-surgery.
POST SURGICAL REHABILITATION
Post-operative knee rehabilitation is one of the most important aspects of knee surgery. The most successful and quickest outcomes result from the guidance and supervision of an experienced sports physiotherapist.
Your physiotherapy rehabilitation following knee surgery focuses on restoring full knee motion, strength, power and endurance. You'll also require balance, proprioception and agility retraining that is individualised towards your specific sporting or functional needs.
As mentioned earlier your sports physiotherapist is an expert in this field. We suggest you contact them for the best advice in your circumstances.
Your physiotherapist will guide your return to sport. It is highly variable and depends upon on your specific knee ligament injury and the demands of your demands of your sports.
PREVENTION OF RECURRENCE
A knee strengthening, agility and proprioceptive training program is the best way to reduce your chance of a knee ligament sprain. Premature return to high-risk activities such as sport are best discussed with your physiotherapist or surgeon.
Other Related Post :


No comments:
Post a Comment